Fundamentals of Nursing serves as a comprehensive guide, outlining the core principles, concepts, and skills essential for effective nursing practice. It covers the roles and responsibilities of nurses, the healthcare environment, and the application of evidence-based practice. The text emphasizes critical thinking, patient-centered care, and the nursing process, providing a solid foundation for nursing education and practice across diverse settings.
1;1 Overview of Nursing Fundamentals
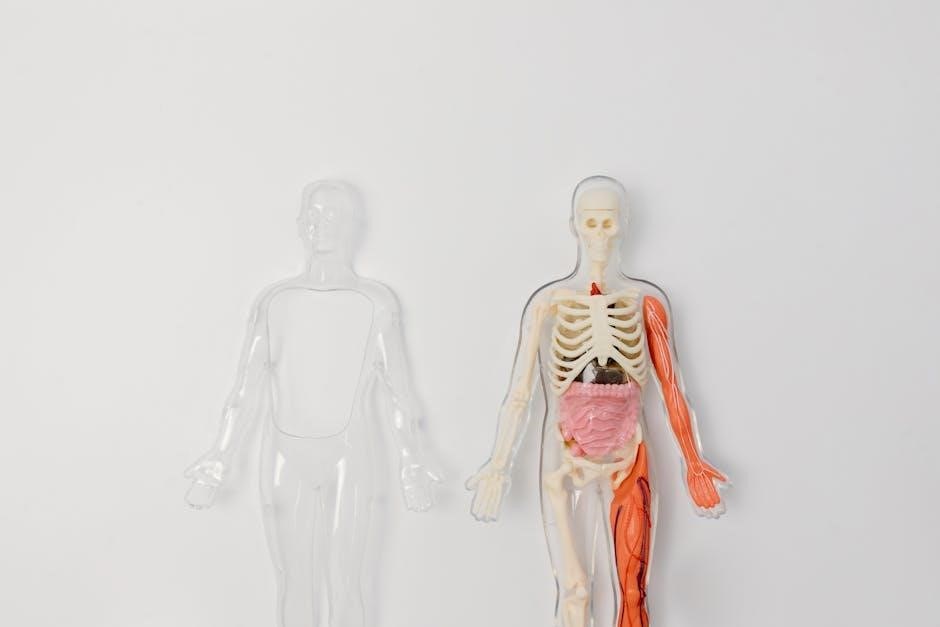
Nursing fundamentals encompass the basic principles, skills, and practices essential for quality patient care. They include patient assessment, communication, infection control, and ethical considerations. These foundational concepts ensure safety, comfort, and holistic care, forming the backbone of nursing practice across diverse healthcare settings.
1.2 Importance of Evidence-Based Practice in Nursing
Evidence-based practice integrates best research evidence, clinical expertise, and patient preferences to guide nursing decisions. It enhances patient outcomes, reduces errors, and promotes cost-effective care. By adhering to evidence-based guidelines, nurses deliver high-quality, standardized care, ensuring safety and improving healthcare systems.

The Nursing Process
The nursing process is a systematic, patient-centered approach to care, emphasizing assessment, diagnosis, planning, implementation, and evaluation. It ensures individualized, evidence-based care.
2.1 Assessment in Nursing Care
Assessment in nursing care involves gathering comprehensive data about a patient’s physical, emotional, and social status. This step uses observation, interviews, and physical examinations to identify health needs and risks, ensuring personalized care plans. Accurate assessment is crucial for effective care delivery.
2.2 Nursing Diagnosis and Planning
Nursing diagnosis identifies health issues or risk factors, enabling the development of individualized care plans. This step involves defining measurable goals and interventions based on evidence-based practices. Effective planning ensures the delivery of targeted care, promoting positive patient outcomes and addressing specific needs systematically.
2.3 Implementation of Nursing Care
Implementation involves executing the care plan through interventions tailored to the patient’s needs. Nurses administer medications, perform procedures, and provide education. This phase requires effective communication and collaboration with the healthcare team to ensure safe, ethical, and evidence-based care, promoting optimal patient outcomes and adapting strategies as needed.
2.4 Evaluation of Nursing Outcomes
Evaluation assesses the effectiveness of care by comparing patient outcomes with established goals. Nurses measure progress, identify unmet needs, and modify care plans accordingly. This phase ensures accountability, reflects evidence-based practices, and highlights the impact of nursing interventions on patient well-being, fostering continuous improvement in care delivery and patient satisfaction.

Core Concepts and Skills in Nursing
Core concepts in nursing include patient-centered care, effective communication, and infection control. Essential skills involve assessing vital signs, ensuring safety, and providing compassionate, evidence-based care.
3.1 Patient-Centered Care and Communication
Patient-centered care focuses on respecting patients’ preferences, values, and needs. Effective communication involves active listening, empathy, and clear expression. Nurses use therapeutic techniques to build trust, ensure understanding, and involve patients in care decisions, fostering a collaborative and supportive environment that enhances health outcomes and patient satisfaction. This approach is integral to holistic nursing practice.
3.2 Infection Control and Safety Measures
Infection control is critical for preventing the spread of pathogens. Nurses use hand hygiene, personal protective equipment, and sterilization techniques to ensure patient safety. Safety measures include proper waste disposal, sharps management, and adherence to isolation protocols. These practices minimize healthcare-associated infections and maintain a safe environment for both patients and healthcare providers, promoting high-quality care delivery.
3.3 Vital Signs and Basic Assessment Techniques
Accurate measurement of vital signs, including temperature, pulse, respiration, and blood pressure, is essential for assessing patient health. Nurses also perform basic assessments, such as observing physical condition, monitoring oxygen saturation, and evaluating pain levels. These techniques provide baseline data, guide care decisions, and help detect deviations from normal, ensuring timely interventions and promoting optimal patient outcomes effectively.

Legal and Ethical Considerations in Nursing
Nursing practice is guided by legal standards and ethical principles, ensuring patient rights, confidentiality, and informed consent. These frameworks protect both patients and nurses, promoting trust and integrity.
4.1 Professional Standards and Codes of Conduct
Professional standards and codes of conduct in nursing establish ethical guidelines and legal obligations, ensuring accountability and respect for patient rights. These frameworks promote integrity, confidentiality, and compassion, guiding nurses to deliver high-quality care while upholding the profession’s values and maintaining public trust.
4.2 Patient Confidentiality and Privacy
Patient confidentiality and privacy are fundamental ethical and legal obligations in nursing. Nurses must protect patients’ personal and medical information, adhering to laws like HIPAA. Breaches of confidentiality can erode trust and lead to legal consequences, emphasizing the importance of strict adherence to privacy protocols in all healthcare settings.
4.3 Informed Consent and Ethical Decision-Making
Informed consent ensures patients are fully aware of their treatment options, risks, and benefits, enabling autonomous decisions. Ethical decision-making in nursing involves respecting patient autonomy, dignity, and rights, while adhering to professional standards and legal requirements. Nurses must navigate complex situations with empathy and integrity, ensuring care aligns with patients’ values and best interests.

Role of Communication in Nursing Practice
Effective communication is vital in nursing, enhancing patient care and outcomes. It supports collaboration, empathy, and clear information exchange, fostering trust and teamwork in healthcare settings.
5.1 Therapeutic Communication Techniques
Therapeutic communication techniques, such as active listening, empathy, and validation, are essential in nursing. These methods foster trust and understanding, enabling nurses to address patients’ emotional and psychological needs effectively. Open-ended questions and non-verbal cues enhance patient engagement, promoting a supportive environment for care. These skills are critical for building strong nurse-patient relationships and improving health outcomes.
5.2 Interdisciplinary Collaboration and Teamwork
Interdisciplinary collaboration in nursing involves teamwork among healthcare professionals to provide comprehensive patient care. Effective communication and mutual respect are crucial for coordination. This approach enhances patient outcomes by combining diverse expertise. It fosters a supportive environment, reduces medical errors, and improves job satisfaction among healthcare providers, leading to higher quality care and better patient experiences.

Safety in Nursing Practice
Safety in nursing practice focuses on preventing harm to patients, healthcare workers, and environments. It involves patient safety protocols, risk management, safe medication administration, and proper handling techniques to minimize errors and enhance care quality.
6.1 Patient Safety and Risk Management
Patient safety and risk management are critical in nursing to prevent harm and ensure high-quality care. Nurses identify potential risks, implement safety measures, and report incidents to improve outcomes. Effective strategies include using evidence-based practices, adhering to safety guidelines, and fostering a culture of safety within healthcare settings to protect patients and reduce adverse events.
6.2 Medication Safety and Administration
Medication safety and administration are critical tasks in nursing to prevent errors and ensure therapeutic effectiveness. Nurses follow the “5 rights” (right patient, drug, dose, time, and route) and use technologies like barcode scanning to enhance accuracy. Proper documentation, patient education, and adherence to policies are essential to minimize adverse events and promote safe medication practices.
6.3 Safe Handling and Mobility Techniques
Safe handling and mobility techniques are essential to prevent injuries and ensure patient safety. Nurses use mechanical aids like slings or lifts and ergonomic manual techniques. Proper assessment of the patient’s condition is crucial. Training in these methods and adherence to established protocols minimize risks for both patients and healthcare providers effectively.
Cultural Competence in Nursing
Cultural competence in nursing involves understanding and respecting diverse patient backgrounds to provide individualized care. It emphasizes effective communication, addressing health disparities, and delivering patient-centered care.
7.1 Understanding Cultural Diversity in Healthcare
Cultural diversity in healthcare requires nurses to recognize and respect patients’ varied beliefs, values, and practices. This understanding ensures personalized care, improves communication, and addresses disparities. Nurses must stay informed about cultural differences to provide sensitive and effective care across diverse populations, fostering trust and better health outcomes for all patients.
7.2 Providing Care to Diverse Patient Populations
Providing care to diverse populations involves tailoring nursing practices to meet the unique needs of individuals from varied cultural, ethnic, and social backgrounds. Nurses must adapt communication strategies, respect cultural practices, and address language barriers to deliver equitable care. This approach ensures high-quality, patient-centered care that respects individual differences and promotes positive health outcomes.
7.3 Addressing Health Disparities and Inclusivity
Addressing health disparities requires nurses to identify and mitigate inequities in healthcare access and outcomes. Inclusivity involves respecting diverse patient values, beliefs, and cultural practices. Nurses must advocate for equitable care, ensuring all patients receive tailored, evidence-based interventions. This approach fosters trust, improves health outcomes, and promotes social justice in healthcare settings.

Nursing Care Plans and Documentation
Nursing care plans and documentation are essential for delivering systematic, patient-centered care. They ensure continuity, accountability, and legal compliance, while promoting evidence-based practice and improved patient outcomes.
8.1 Developing Effective Care Plans
Developing effective care plans involves using assessment data to create patient-centered goals and interventions. Plans should be clear, measurable, and time-bound, ensuring individualized care. Collaboration with the healthcare team is crucial for consistency and optimal outcomes, aligning with evidence-based practices to promote safety and efficiency in care delivery.
8.2 Accurate Documentation and Reporting
Accurate documentation and reporting are critical for maintaining patient safety and continuity of care. Clear, concise records ensure accountability and effective communication among healthcare providers. Standardized formats and legal guidelines must be followed to maintain confidentiality and integrity of patient information, supporting evidence-based practice and informed decision-making in nursing care delivery.

Technology in Nursing Practice
Technology in nursing enhances patient care through tools like EHRs, telehealth, and mobile apps, improving communication and data accessibility. It streamlines workflows, supports evidence-based practice, and ensures patient confidentiality, fostering safer and more efficient care delivery.
9.1 Electronic Health Records (EHRs) and Nursing Informatics
Electronic Health Records (EHRs) and Nursing Informatics are integral to modern nursing, enhancing accuracy, accessibility, and efficiency in patient care. EHRs streamline documentation, improve data organization, and facilitate communication among healthcare providers. Nursing Informatics supports evidence-based practice through tools like MyLab Nursing and resources on the Evolve website, aiding nurses in delivering high-quality, data-driven care while maintaining patient confidentiality and care coordination.
9.2 Telehealth and Remote Nursing Care
Telehealth and remote nursing care have revolutionized healthcare delivery, enabling nurses to provide patient care from a distance. Through digital platforms, nurses can monitor patients, conduct virtual consultations, and educate patients on self-care. Telehealth enhances accessibility, reduces costs, and improves continuity of care, especially for rural or underserved populations, while maintaining high-quality, patient-centered nursing services. This approach is increasingly vital in modern healthcare systems.

Professional Development in Nursing
Professional development in nursing emphasizes continuing education, lifelong learning, leadership roles, and mentorship. It utilizes dynamic study tools, NCLEX reviews, and case studies, supported by expert authors for career advancement.
10.1 Continuing Education and Lifelong Learning
Continuing education and lifelong learning are vital for nursing professionals, ensuring they stay updated with evidence-based practices and industry advancements. Textbooks, online platforms like MyLab Nursing, and resources such as Evolve support ongoing education. These tools provide dynamic study modules, case studies, and NCLEX review questions, fostering professional growth and adaptability in the evolving healthcare landscape.
10.2 Leadership Roles and Mentorship in Nursing
Leadership roles in nursing involve guiding teams, influencing care quality, and advocating for patient well-being. Mentorship fosters professional growth by pairing experienced nurses with newcomers, enhancing skills and confidence. Effective leadership and mentorship are crucial for fostering a supportive environment, promoting evidence-based practices, and advancing the nursing profession. These roles are essential for driving positive outcomes in healthcare settings.